
In January 2025, the Texas Department of State Health Services (DSHS) identified the first measles cases in a West Texas outbreak. On August 18, DSHS declared the outbreak in Texas over after 42 days without new cases; Texas’ final totals are 762 cases, 99 hospitalizations, and two deaths in school-aged children. The Texas outbreak was linked with outbreaks in New Mexico, Oklahoma, and Kansas. As of August 21, the Kansas Department of Health and Environment reports 87 confirmed cases, 8 hospitalizations, and has also declared its outbreak over. As of August 28, the New Mexico Department of Health reports 100 cases statewide. As of August 26, the Oklahoma State Department of Health lists 20 total cases (17 confirmed, 3 probable) and no deaths.
Texas reported its first death on February 26 (an unvaccinated school-aged child with no known underlying conditions), and a second on April 6, also an unvaccinated school-aged child. New Mexico reported on March 6 that an unvaccinated adult who died had tested positive for measles (cause of death under investigation).
Measles was declared eliminated from the U.S. in 2000 (elimination is defined by the CDC as the absence of endemic measles virus transmission in a region for at least 12 months). However, due to declining vaccination rates, the number of outbreaks has increased in recent years. Large outbreaks can occur when an individual infected with measles (who may have been infected through travel to or from a high prevalence area) introduces the virus into an under-vaccinated community.
Measles is one of the most infectious viruses known; each infected person will infect 15 to 18 other susceptible individuals. The measles virus is spread through the air when an infected person coughs or sneezes. You can get measles either through direct contact with an infected person or simply by entering a room up to two hours after a person with measles has left that same room. Measles is only spread from person to person. If one person has measles, up to 90% of the people close to them will develop measles if they are not protected by vaccination or prior infection. Outbreaks are most common in late winter and spring.
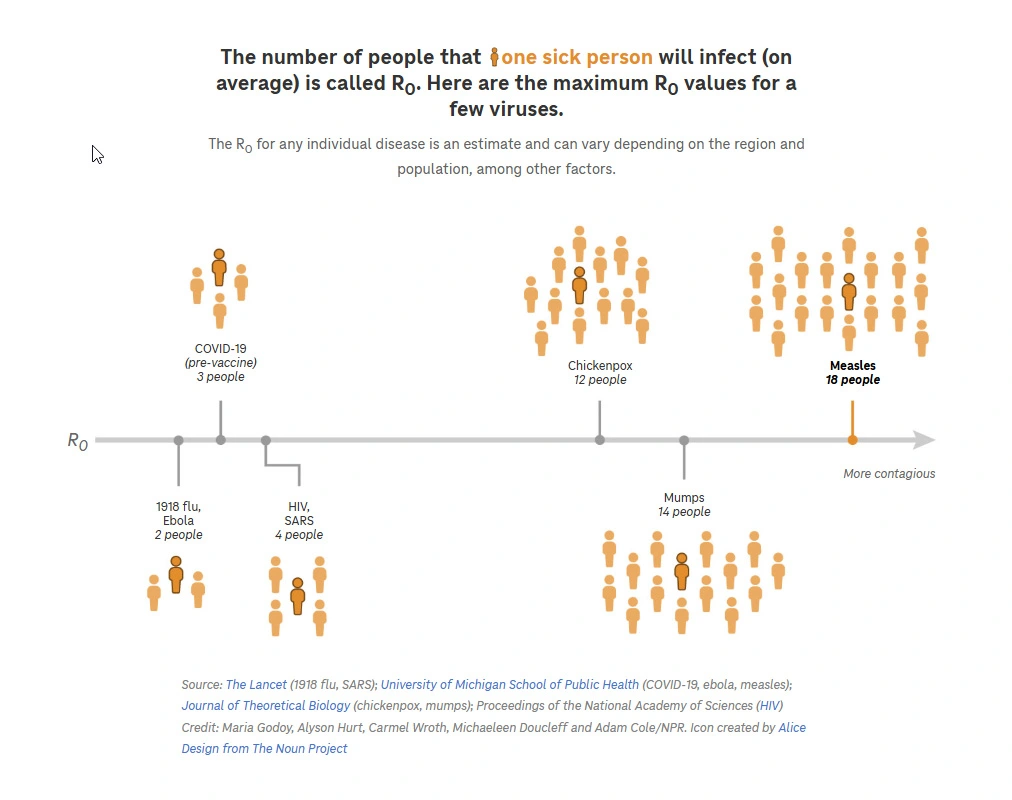
Source: NPR Houston Public Media
Measles symptoms appear 7 to 14 days after infection. Common symptoms include:
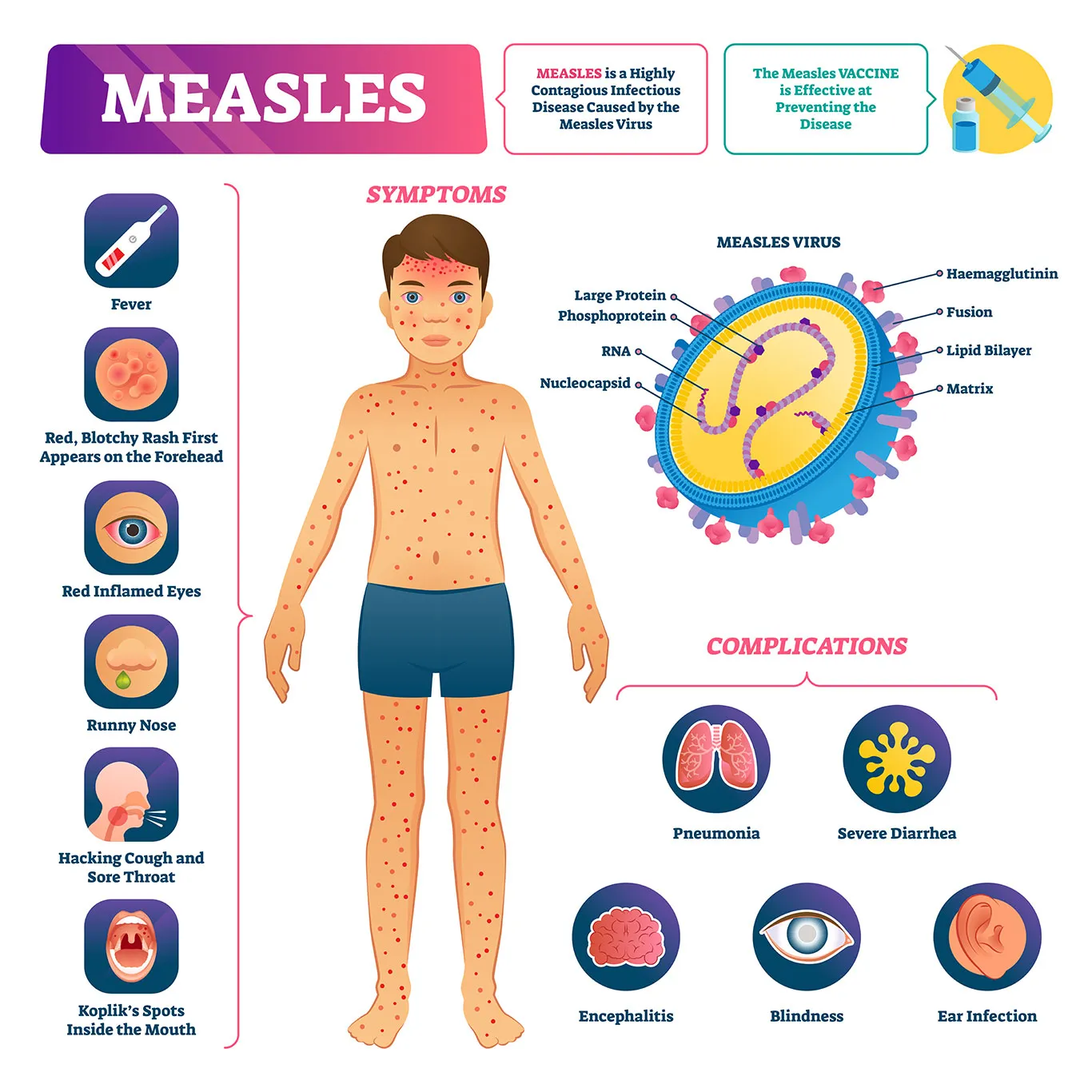
Measles is not a harmless disease. While common complications are ear infections and diarrhea, severe complications can include pneumonia and encephalitis (inflammation of the brain), the latter potentially causing permanent brain damage. The virus can also cause direct damage to the inner ear, leading to permanent deafness.
One to three of every 1,000 children infected with measles virus will die from its complications. One out of five people with measles require hospitalization, and this number increases to over half for children who are under 5 years old.
Subacute sclerosing panencephalitis (SSPE) is a rare form of progressive brain inflammation and is nearly always fatal. SSPE develops in approximately 4 to 11 out of every 100,000 measles cases. The risk is higher (18 per 100,000 cases) among children infected before the age of five.
Anyone who is not protected against measles (by vaccination or prior infection) is at risk of infection. Groups at higher risk of severe disease include:
There is no specific antiviral treatment available.
Supportive care includes fluids (staying hydrated), rest, and taking acetaminophen to manage fever and pain. Vitamin A supplements may be recommended.
Vaccination is the best way to prevent infection, either with the MMR (measles, mumps, rubella) or MMRV (measles, mumps, rubella, varicella) vaccine. Two doses of vaccine are needed for the best protection. The current recommended vaccination schedule typically advises administering the MMR vaccine to children at 15-18 months of age. However, in certain situations, it can be given as early as 6 months. Parents should consult with their pediatrician to determine the most appropriate time for their child's vaccination.
An additional dose of the vaccine is recommended for those born between 1957 and 1968, as this group may have received a version of the vaccine that was less effective. Those born before 1957 are presumed to be immune from prior measles infection. If you are unsure about your vaccine status, check your healthcare or school records, or consult with your health care provider. Antibody levels also can be tested to determine immunity.
Infected individuals should be isolated, although they can transmit the virus before showing any symptoms. To safeguard immunocompromised individuals, as well as newborns under 6 months old, who cannot be vaccinated, it is crucial that their close contacts receive the vaccine.
Postexposure prophylaxis for unvaccinated individuals:
Recommendations for Healthcare Providers
Recommendations for Healthcare Departments
Recommendations for Travelers